MIPS Basics
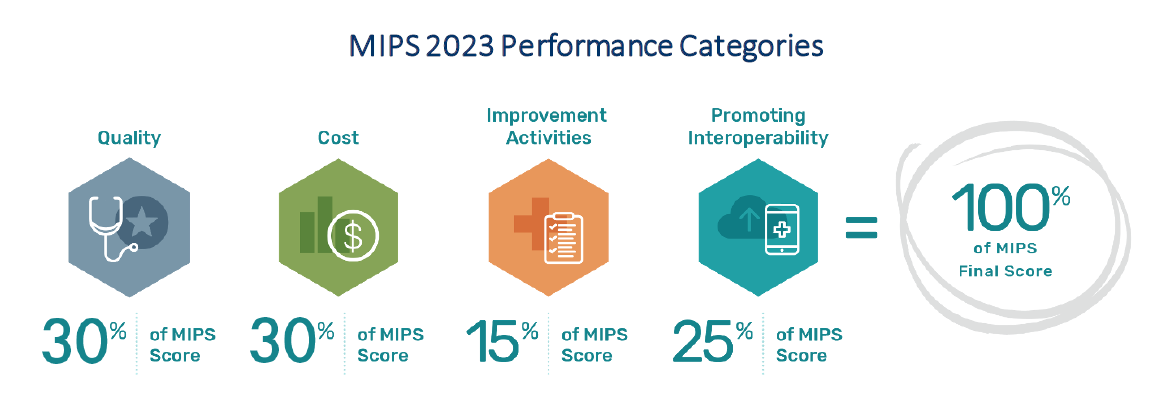
There are 4 performance categories again for 2023. The points from each category are added together to give you a MIPS score. The 2023 MIPS performance period is from January 1, 2023, to December 31, 2023. Following the performance period, if you submit 2023 date for MIPS, the deadline is March 31, 2024. Your MIPS final score is compared to the MIPS performance threshold to determine if you receive a positive, negative, or neutral payment adjustment in the 2025 payment year.
2023 Quality Requirements
This percentage can change due to Special Statuses, Hardship Exception Applications, reweighting of other performance categories, or Alternative Payment Model (APM) participation.
2023 MIP Quality Performance Category – 30%
Participants must collect measure data for the 12-month performance period (January 1 - December 31, 2023). The amount of data that must be submitted depends on the collection (measure) type.
There are 5 collection types for quality measures:
- Electronic Clinical Quality Measures (eCQMs),
- MIPS Clinical Quality Measures (CQMs),
- Qualified Clinical Data Registry (QCDR) Measures,
- Medicare Part B claims measures,
- The Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS Survey
NOTE: CMS Web interface is no longer available as a collection or submission type for groups, virtual groups, and APM Entities participating in traditional MIPS starting with 2023 performance year.
General reporting requirements:
- You will typically need to submit collected data for at least 5 measures (including 1 outcome measure or high-priority measure in the absence of an applicable outcome measure), or a complete specialty measure set.
- You will need to report performance data for 70% of the patients who qualify for each measure (data completeness).
- You can submit measures from different collection types (except CMS Web Interface measures) to fulfill the requirement to report 5 measures.
- 20 case minimum on each measure.
Quality Improvement Score
Individual MIPS eligible clinicians, groups, virtual groups, and APM Entities may earn up to 10 additional percentage points based on your improvement in the quality performance category from the previous year.
How Should I Submit Data?
There are 3 submission types you can use for quality measures. The submission types are:
- Medicare Part B claims (small practices only)
- Sign in and upload
- Direct submission via Application Programming Interface (API)
Bonus Points
Bonus points are only available for small practices. Six bonus points will continue to be added to the quality performance category score for clinicians in small practices who submit at least one measure, either individually or as a group, virtual group, or APM Entity. Such bonus isn’t added to clinicians or groups who are scored under facility-based scoring.
2023 PI Requirements – 25%
This percentage can change due to special statuses, hardship exception applications, or Alternative Payment Model (APM) Entity participation.
Requirements
For the 2023 performance year, you’re required to use an Electronic Health Record (EHR) that meets the 2015 Edition Cures Update certification criteria for participation in this performance category.
You must submit collected data for the required measures in each objective (unless an applicable exclusion is claimed) for the same 90 continuous days (or more) during 2023.
In addition to submitting measures, you must provide your EHR’s CMS Identification code from the Certified Health IT Product List (CHPL) and submit a “yes” to:
- The Actions to Limit or Restrict Compatibility or Interoperability of CEHRT (previously named the Prevention of Information Blocking) Attestation.
- The Office of the National Coordinator for Health Information Technology (ONC) Direct Review Attestation.
- The Security Risk Analysis Measure.
- The Safety Assurance Factors for EHR Resilience (SAFER) Guides Measure (a "no" will also satisfy this measure).
Who is required to report PI Data?
There are several clinician types and special status designations that result in automatic reweighting. These clinicians, groups, virtual groups, and APM Entities are exempt from reporting Promoting Interoperability data for the 2023 performance year:
Beginning with the 2023 performance year, some clinician types will no longer be automatically reweighted and are therefore required to report Promoting Interoperability data:
Hardship Exceptions
Individuals, groups, and virtual groups may submit a MIPS Promoting Interoperability Performance Category Hardship Exception application, citing one of the following reasons for review and approval:
- MIPS eligible clinician using decertified EHR technology
- Insufficient Internet connectivity
- Extreme and uncontrollable circumstances
- Lack of control over the availability of CEHRT
If your hardship exception is approved, the Promoting Interoperability performance category will receive zero weight when calculating your final score and the 25% will be redistributed to another performance category (or categories) unless you submit data for this performance category.
How Should I Submit Data?
There are 3 submission types you can use for your Promoting Interoperability performance category data, depending on which submitter type you are. The submission types are:
- Sign in and attest
- Sign in and upload
- Direct submission via Application Programming Interface (API)
Bonus Points
You can earn 5 bonus points for submitting a "yes" response for one of the optional Public Health and Clinical Data Exchange measures (Public Health Registry Reporting, Clinical Data Registry Reporting, or Syndromic Surveillance Reporting).
Beginning with the 2023 performance year, there are no bonus points available for the Query of Prescription Drug Monitoring Program (PDMP) measure since this measure is now required.
2023 Improvement Activities Requirement – 15%
This percentage can change due to special statuses, exception applications or Alternative Payment Model (APM) Entity participation.
What Improvement Activities Data Should I Submit?
To earn full credit in this performance category, you must generally submit one of the following combinations of activities:
- 2 high-weighted activities
- 1 high-weighted activity and 2 medium-weighted activities, or
- 4 medium-weighted activities
Improvement activities have a continuous 90-day performance period (during CY 2023) unless otherwise stated in the activity description.
UPDATED For group reporting, a group or virtual group can attest to an activity when at least 50% of the clinicians in the group or virtual group perform the same activity during any continuous 90-day period (or as specified in the activity description) in the same performance year.
How Should I Submit Data?
There are 3 submission types you can use for Improvement Activities, depending on which submitter type you are. The submission types are:
- Sign in and attest
- Sign in and upload
- Direct submission via Application Programming Interface (API)
2023 Cost Requirements – 30%
This percentage can change due to exception applications, Alternative Payment Model (APM) Entity participation, or if you don’t meet the established case minimum for at least one cost measure. If you don't meet the established case minimum for any of the available cost measures, the cost performance category will receive zero weight when calculating your final score and the 30% will be distributed to another performance category (or categories).
There are 25 cost measures available for the 2023 performance period, including:
- Episode-based cost measures based on a range of procedures, acute inpatient medical conditions, and chronic conditions, and
- Population-based cost measures focused more broadly on primary and inpatient care.
NOTE: The cost performance category is weighted to 0% for MIPS APM Entities that choose to report traditional MIPS.
What Cost Data Should I Submit?
We use Medicare administrative claims data to calculate cost measure performance, which means clinicians and groups don’t have to submit any data for this performance category.
UPDATED Improvement Scoring
Starting with the calendar year 2022 performance period/2024 MIPS payment year, we’ve established a maximum cost improvement score of 1 percentage point out of 100 percentage points available for the cost performance category.
NOTE: All MIPS eligible clinicians will receive a cost improvement score of zero percentage points for the 2022 performance period because we didn’t calculate cost measure scores for the 2021 performance period.